Image credit: naitbabies.org
Families Share Their FNAIT Journeys, and Hope for a New Treatment in Clinical Trial:
The McGrew Family Story: When Your Baby Has FNAIT
Briana Gray’s FNAIT Story of Triumph and Advocacy
FNAIT Research: Evaluating and Investigational Medication
What is FNAIT or NAIT?
Fetal and Neonatal Alloimmune Thrombocytopenia (FNAIT, pronounced “F Nate”), also known as Neonatal Alloimmune Thrombocytopenia (NAIT, “Nate”), is a rare pregnancy-related disorder characterized by a low fetal blood platelet count that affects babies in utero or immediately after birth. Platelets are crucial in the prevention of bleeding. While some cases of FNAIT may present with mild symptoms, the spectrum of effects can vary significantly, ranging from a low platelet count without symptoms to severe bleeding into the brain that can become fatal.
Prevalence of FNAIT:
According to National Organization for Rare Disorders, approximately one in 1,500 pregnancies are affected by FNAIT.
Causes of FNAIT:
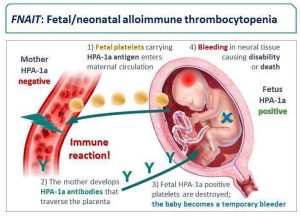
The onset of decreased platelet count begins during pregnancy when there is an incompatibility between the mother’s platelet type and the baby’s platelet type. The incompatibility occurs because of a protein or antigen found on the surface of the platelet that is inherited from the father. The usual platelet antibody is called anti-HPA-1a although cases with anti-HPA-5b can also cause FNAIT.
In such instances, when the baby’s blood encounters the mother’s blood through the placenta, the mother’s immune system mistakenly recognizes the platelets as foreign entities and mounts an immune response by producing antibodies that move back across the placenta and attack and eliminate the fetal platelets.
The infant’s resulting insufficient supply of platelets to prevent bleeding means that even minor injuries can have serious consequences.
Symptoms of FNAIT:
In mild cases, skin discolorations called petechiae and purpura, caused by bleeding under the skin or severe bruising can occur within a few hours of birth.
In more severe cases, bleeding in critical areas such as the intestines, lungs, or eyes can pose serious risks. The most severe symptom is brain bleeding (intracranial hemorrhage or ICH) which can cause brain damage or death.
Diagnosis of FNAIT:
Most cases of FNAIT remain undetected until birth when symptoms become apparent. Once symptoms appear, a test of the baby’s blood is typically performed to determine the platelet count. Ultrasound may also be used to see if bleeding has taken place in the brain. Additionally, the mother’s blood is screened for the presence of specific antibodies to the baby’s platelets.
Screening for FNAIT is typically considered only if the condition is suspected when an older sibling from a previous pregnancy had a bleeding problem before or after birth. Therefore, due to the lack of routine screening in pregnancy, FNAIT is often underdiagnosed.
Treatment of FNAIT:
The current standard of care is the use of intravenous immunoglobulin therapy with or without oral corticosteroids given to the mother during pregnancy.
Experimental approaches are being studied to reduce the level of antibodies in the mother’s bloodstream and to block the passage of platelets across the placenta that attack the baby’s platelets. Learn more from the resources listed below.
Prognosis of FNAIT:
Milder cases of FNAIT typically resolve in 2 to 6 weeks after birth. More severe cases can experience lifelong damage or death.
